Some facts about the disease:
Osteochondrosis of the neck occurs in men and women approximately equally.
What characteristics of the cervical spine cause the symptoms of osteochondrosis?
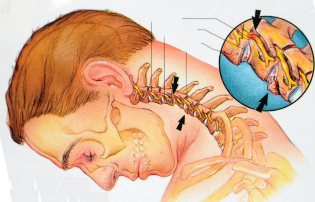
- There are openings in the lateral processes of the vertebrae - through them the carotid arteries pass through them to the right and left, which supply the brain.
- The initial part of the spinal cord passes through the cervical region - it contains fibers that bring nerve impulses to all parts of the body, provide movement, sensitivity. If there is spinal cord compression in the neck, neurological disorders occur throughout the body.
- This part of the spine has a lot of mobility and this predisposes to osteochondrosis (although, in most cases, the disease still develops in the lumbar spine - not only does it have high mobility, but it also experiences the greatest stress).
- In the cervical area, the nerve roots emerge from the intervertebral foramen, forming the cervical and brachial plexus. They are responsible for movements in the muscles of the neck, arms, shoulder girdle, skin sensitivity and regulation of autonomic functions.
- The first vertebra does not have a massive anterior part - a body - it is a bone ring that is put in a tooth - a bony protrusion in the second vertebra. Thanks to this, head turns on the sides are possible.
Neck pain, headaches, feeling weak, numbness in the hands are symptoms that should force you to see a neurologist. Examination by a specialist and examination using modern equipment will help to understand the causes of the pathology and take the most effective measures.
What happens to the vertebrae in cervical osteochondrosis?
The ambiguous medical term "degenerative process" refers to the following pathological changes that occur in the cervical spine:
- First of all, osteochondrosis damage covers the intervertebral discs. They become thinner, thus reducing the distance between adjacent beads. Small tears, microcracks form on their outside. Over time, this can lead to a herniated disc.
- As a result of disc damage, the stability of the vertebral joint is broken.
- They suffer from osteochondrosis of the cervical spine and intervertebral joints - spondyloarthritis develops. It also contributes to the compression of nerve roots.
- The pathological process extends to the vertebrae themselves. Due to the fact that the functions of the intervertebral discs are disrupted, the load on them increases. The spine is trying to compensate for this violation, bone outgrowths - osteophytes - appear in it.
Treatment of cervical spine osteochondrosis
During an exacerbation of cervical vertebral osteochondrosis, traction is used (the patient is placed on a bed with a raised forehead and the head is fixed with a special loop) to facilitate the intervertebral discs. For the same purpose, you should wear a Shants collar. Pain relievers and anti-inflammatory drugs are prescribed for pain relief. In case of a strong pain that does not disappear in any way, the doctor may block: inject an anesthetic solution into the area of the affected nerve roots. Physiotherapy used: ultrasound treatment, novocaine electrophoresis.
When the deterioration subsides, the treatment of osteochondrosis of the cervical spine includes massage, physiotherapy exercises, physiotherapy.
One of the main signs of cervical osteochondrosis is neck pain. Many people who are faced with this symptom do not go to the doctor but prefer to treat chondrosis with home methods. There are at least two good reasons to refuse self-medication and consult a specialist doctor.
First, pain relievers and popular methods, although they help relieve pain for a while, do not solve the main problem. Pathological changes in the spine continue to grow. Over time, this threatens more serious consequences. To the point that surgery may be required.
Second, neck pain occurs not only with osteochondrosis. There are many other reasons. Only a doctor can understand and prescribe the right treatment.
What symptoms of cervical spine osteochondrosis should make you see a doctor?
The main symptom of cervical osteochondrosis is pain. It can occur in different places, depending on the level at which the pathological process is localized: in the neck, in the shoulder girdle, in the hand, in the region of the heart. By nature, the pain is dull, it may be burning, it hurts.
Other manifestations of the disease:
- Headache, dizziness, flies in front of eyes, noise, tinnitus.
- Weakness in neck muscles, shoulder girdle, arms.
- Disorder of skin sensitivity.
- Shoulder-shoulder periarthritis: neck pain extending to the arm, difficulty grasping the arm above 90 °, weakness and atrophy of the shoulder girdle muscles.
- Shoulder Hand Syndrome: shoulder and hand pain, swelling and stiffness of the fingers, weakness and atrophy of the hand muscles.
- Vertebral artery syndrome. Bone growths appear in the vertebrae, which squeeze the nerves, resulting in a reflex spasm of the vertebral artery, which participates in the blood supply to the brain. Symptoms of cervical osteochondrosis are accompanied by persistent headaches starting from the back of the head, spreading to the temple, crown, nausea, ringing in the ears, ringing in the ears, trembling of bright spots in front of the eyes.
- Anterior degree muscle syndrome. In the neck there are anterior and middle muscles - they are located next to each other, and between them there is a small space in which nerves and blood vessels pass. With osteochondrosis of the cervical spine, the sciatic anterior muscles tense and tighten them, resulting in symptoms such as pain on the inner surface of the forearm, shoulder, and fingers. Sometimes the pain radiates to the back of the head. The skin of the hand may become cold, pale and numbness may appear.
- Epicondylitis syndrome. In the lower part of the shoulder, on the sides of the elbow joint, there are bony-epicondyle extensions. With epicondylitis syndrome caused by cervical osteochondrosis, they experience pain, which intensifies when pressed. Other symptoms also occur: neck pain, soreness when pressing certain points on the vertebrae of the cervix.
If two parts of the spine are affected at the same time, with cervicothoracic osteochondrosis, symptoms may include pain between the shoulder blades, in the heart region.
With osteochondrosis, the risk of intervertebral hernia and stroke increases. If you experience the symptoms listed above, see your doctor.
It's better not to treat yourself. Even if you have proven and true methods that can usually help you manage your pain, it does not mean that you are doing it right.
Pain can be caused not only by osteochondrosis, but also by intervertebral hernia, muscle disorders (myofascial pain syndrome) and be a symptom of other diseases. To properly treat the disease, you need to understand its causes, make differential diagnoses. This is only possible in one clinic.
To identify the cause of the disease and to accurately treat the symptoms of cervical osteochondrosis, you should visit a neurologist, undergo an examination.
At the heart of cervical osteochondrosis is the defeat of the intervertebral discs. Their chemical composition is violated, at first they swell, then shrink in size, cracks and tears appear on their outside, they become denser. The degenerative process then spreads to the vertebrae, the intervertebral joints. Due to a decrease in the height of the intervertebral disc, the load on the vertebrae increases, and bone growths appear in them - osteophytes.
What are the causes of cervical spine osteochondrosis?
There is no consensus on the causes of cervical osteochondrosis. Different conditions are thought to cause disease, there are different perspectives:
- Age-related changes in the spine. However, almost all people over the age of 40 have skeletal changes, but not all have osteochondrosis.
- Neck Injuries. Often among the causes of the disease, trauma is indicated: a bruised neck, compression fracture, subluxation of the vertebrae. Chronic injuries, such as during intensive training for athletes, persistent uncomfortable bent postures, and repeated whipping injuries in motorists, can be worthwhile.
- Congenital anomalies of the vertebrae: cervical ribs, fusion of adjacent vertebrae, fusion of the first vertebra with the occipital bone, etc.
- Professions. Most often the disease affects people who work in a monotonous behavior, constantly doing the same type of movement.
- Disorder of blood supply to the spine, venous insufficiency, edema in the area of nerve roots.
- Autoimmune disorders.Conditions in which the immune system does not work properly, it attacks its connective tissue, the ligaments of the body.
Visit a neurologist. An experienced healthcare professional will understand the source of your health problems and prescribe the right treatment.
Causes of worsening cervical osteochondrosis
Osteochondrosis persists in the form of alternate exacerbations and periods of improvement, when symptoms cease to bother for a while. Another deterioration can be caused by the following reasons:- Strange and irregular neck movement.
- Long stay in a monotonous uncomfortable position. For example, the neck may start to ache after working at the computer for a long time after sleeping on an uncomfortable pillow.
- Stress, nervous tension. With chronic stress, spasms occur in the neck muscles, this can cause the onset of another deterioration.
- Various diseases, exacerbations of chronic diseases.
- Hypothermia. For this reason, exacerbations in many people occur in the fall.
- Incorrect self-medication, illiterate. For example, massage and therapeutic exercises are helpful during remission but are contraindicated during a deterioration.
Which diseases can have similar manifestations?
Very often the manifestations of "osteochondrosis" are actually associated with a completely different disease. For example, the reason may be hidden in the muscles - there is such a condition as myofascial pain syndrome. The pain arises from the constant tension of the same muscles.
Sometimes the manifestation of "cervical osteochondrosis" is thought to be dizziness associated with otolithiasis - a condition in which crystals of calcium salts accumulate in the inner ear.
Neck pain and seizures, headaches - when these symptoms occur, many people "diagnose" osteochondrosis. Everything is clear - when it hurts, you have to take painkillers or do a ukolchik, put on heat and everything will pass. Why go to the doctor when you can treat it yourself?
However, often self-healing does not lead to anything good. Painful attacks over time can become more frequent, intense, and prolonged. If you take painkillers almost every day, you may have stomach or kidney problems. After all, any medicine has side effects.
And the cause of pain is not always the main cause of osteochondrosis. In order to discover the real cause and understand how to treat it effectively, you need to visit a doctor and undergo an examination.
How does a neurologist diagnose cervical osteochondrosis? What happens in the doctor's office during the examination?
During your first visit, the neurologist will ask you some questions:
- How long have you had a headache, neck pain?
- Where does the pain appear? What kind of character are they: stabbing, pain, shooting, pulling?
- When does pain usually appear? What provokes him? After what do you feel better?
- Have you visited a doctor yet? Have you been examined and treated? What? How long ago?
- What other symptoms are bothering you?
- What other chronic diseases do you have?
- Have you had any neck injuries lately?
Your doctor will do a neurological examination, checking your reflexes, skin sensitivity, muscle strength and tone. You will be asked to turn, tilt your head sideways, forward, backward. The doctor will lightly press your head, at certain points on the neck, to determine the onset of pain.
After the examination, you will be diagnosed and prescribed the necessary diagnostic methods.
What diagnostic methods are used for osteochondrosis of the cervical spine?
Examination for cervical osteochondrosis usually involves the following diagnostic methods:
- Radiography of the cervical spine.
- According to the indications, X-ray contrast studies are described: myelography (introduction of contrast in the space around the spinal cord), discography (introduction of contrast in the intervertebral disc), angiography (introduction of contrast in vessels).
- Computed tomography.
- Magnetic resonance imaging.
- For severe neurological disorders, you may be prescribed electroneuromyography - a study that determines the transmission of electrical impulses to nerves and muscles.
Often, the manifestations of cervical osteochondrosis resemble angina pectoris. If after the examination the doctor still doubts about the diagnosis, you will be prescribed ECG and other diagnostic methods.



































